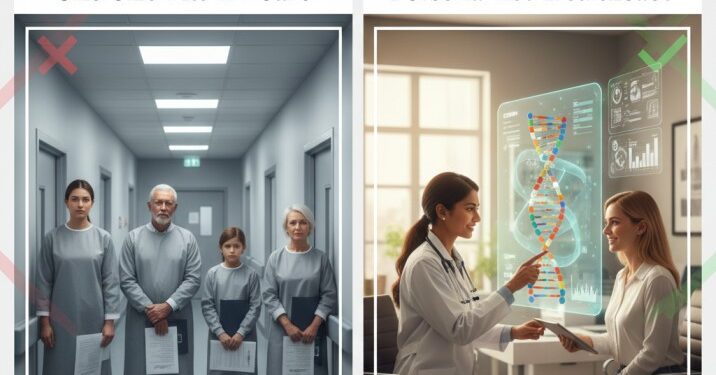
Healthcare has always aimed to treat individuals, yet for much of modern medical history, care has been delivered through standardized pathways. These pathways were designed for efficiency, safety, and population-level outcomes, but they often assumed that patients with similar diagnoses would respond similarly to treatment. In 2026, that assumption is steadily losing ground. Advances in data, technology, and care delivery models are driving a shift toward personalized healthcare, where treatment decisions are increasingly tailored to individual needs rather than averages.
This shift does not mean abandoning clinical guidelines or evidence-based medicine. Instead, it reflects a growing understanding that health outcomes improve when care adapts to the person receiving it. As a result, customized medical care is becoming less of an exception and more of an expectation.
How One-Size-Fits-All Care Became the Standard
To understand why personalized healthcare represents such a meaningful shift, it helps to look at how standardized care models emerged in the first place.
Throughout the twentieth century, healthcare systems expanded rapidly to meet the needs of growing populations. Standardization played a critical role. Clinical protocols helped reduce variation, training became more consistent, and public health outcomes improved. For many acute conditions, standardized treatment pathways saved lives and reduced preventable errors.
However, this approach also had limitations. Patients with the same diagnosis often differed in genetics, lifestyle, environment, and access to care. Standard protocols could not always account for these differences. Over time, this led to a gap between what was clinically recommended and what patients were realistically able to follow or benefit from.
As chronic conditions became more prevalent, these limitations became harder to ignore. Managing long-term health requires ongoing engagement, behavioral changes, and adaptability, areas where rigid care models often struggle.
What Personalized Healthcare Actually Means
Personalized healthcare is sometimes misunderstood as niche or experimental. In practice, it refers to a broad set of approaches that tailor care based on individual characteristics rather than population averages.
At its core, personalized healthcare considers factors such as:
- medical history and comorbidities
- genetics and biomarkers (where relevant)
- lifestyle, habits, and environment
- patient preferences and goals
- response to previous treatments
Rather than asking, “What is the standard treatment for this condition?”, personalized healthcare asks, “What is the most appropriate approach for this person, right now?”
This philosophy does not eliminate guidelines. It refines them. Evidence-based recommendations remain the foundation, but they are applied with flexibility and context.
The Role of Data in Customized Medical Care
The shift toward customized medical care would not be possible without advances in data collection and analysis. Over the last decade, healthcare has gained access to richer and more continuous information about patients.
Digital intake tools capture more detailed histories. Remote monitoring devices provide ongoing data rather than single snapshots. Electronic health records make longitudinal trends easier to identify. Together, these tools allow clinicians to move beyond isolated encounters and toward a more complete picture of patient health.
Data-driven personalization supports:
- earlier identification of risk
- more precise treatment selection
- timely adjustments when plans are not working
- better measurement of outcomes over time
Importantly, personalization does not require complex genetics for every patient. Even simple data points, such as adherence patterns or symptom changes between visits, can meaningfully improve care when used thoughtfully.
Patient Empowerment as a Core Principle
Another reason one-size-fits-all care is fading is a shift in patient expectations. Patients today want to understand their care, participate in decisions, and see how recommendations fit into their lives.
Personalized healthcare supports this by making patients active participants rather than passive recipients. When care plans reflect individual goals and constraints, patients are more likely to engage and follow through.
Empowerment shows up in practical ways:
- care plans explained in plain language
- shared decision-making rather than directive instructions
- follow-up designed around real-world schedules
- feedback loops that allow patients to report progress or challenges
This approach does not undermine clinical authority. It strengthens it by aligning medical expertise with patient reality.
Why Technology Accelerated the Shift
Technology did not create personalized healthcare, but it accelerated its adoption. Virtual care models, digital tools, and telehealth platforms made it easier to deliver customized medical care at scale.
In traditional settings, personalization often depended on time-intensive in-person interactions. Today, technology allows care teams to:
- gather detailed information before visits
- tailor follow-up based on risk level
- adjust care plans without waiting months for the next appointment
- maintain continuity through messaging and monitoring
This scalability is key. Personalized healthcare only works long-term if it can be delivered consistently across diverse populations, not just in boutique settings.
Balancing Personalization With Safety and Consistency
One concern often raised about personalized healthcare is the risk of inconsistency. If care is customized too freely, how do systems ensure safety and quality?
The answer lies in structure. Effective personalized healthcare operates within defined guardrails. Clinical standards still apply, documentation remains rigorous, and escalation pathways are clear. Personalization occurs within these boundaries, not outside them.
In well-designed systems:
- personalization is rule-based, not improvised
- deviations from standard pathways are documented and justified
- outcomes are tracked to ensure changes improve care
- safety mechanisms trigger review when risks increase
This balance allows healthcare to adapt without sacrificing reliability.
Why One-Size-Fits-All Care Is Losing Relevance
The decline of one-size-fits-all care does not reflect a failure of medicine. It reflects progress. As healthcare systems gain better tools, more data, and deeper insight into patient behavior, rigid uniformity becomes less defensible.
Conditions vary. Patients vary. Life circumstances vary. Personalized healthcare acknowledges these realities while preserving the strengths of evidence-based practice.
In 2026, the question is no longer whether customized medical care is possible. It is whether healthcare systems are designed to support it responsibly and at scale.
Conclusion: The Future Is Individual, Not Isolated
Personalized healthcare represents a shift toward care that fits people rather than forcing people to fit care. By combining clinical evidence with individual context, customized medical care improves engagement, outcomes, and trust.
One-size-fits-all models will continue to play a role in acute and emergency care, where speed and standardization are essential. But for long-term health, prevention, and chronic management, personalization is becoming the norm.
The future of healthcare is not about abandoning standards. It is about applying them intelligently, with the individual at the center.